
Importance of Early Diagnosis
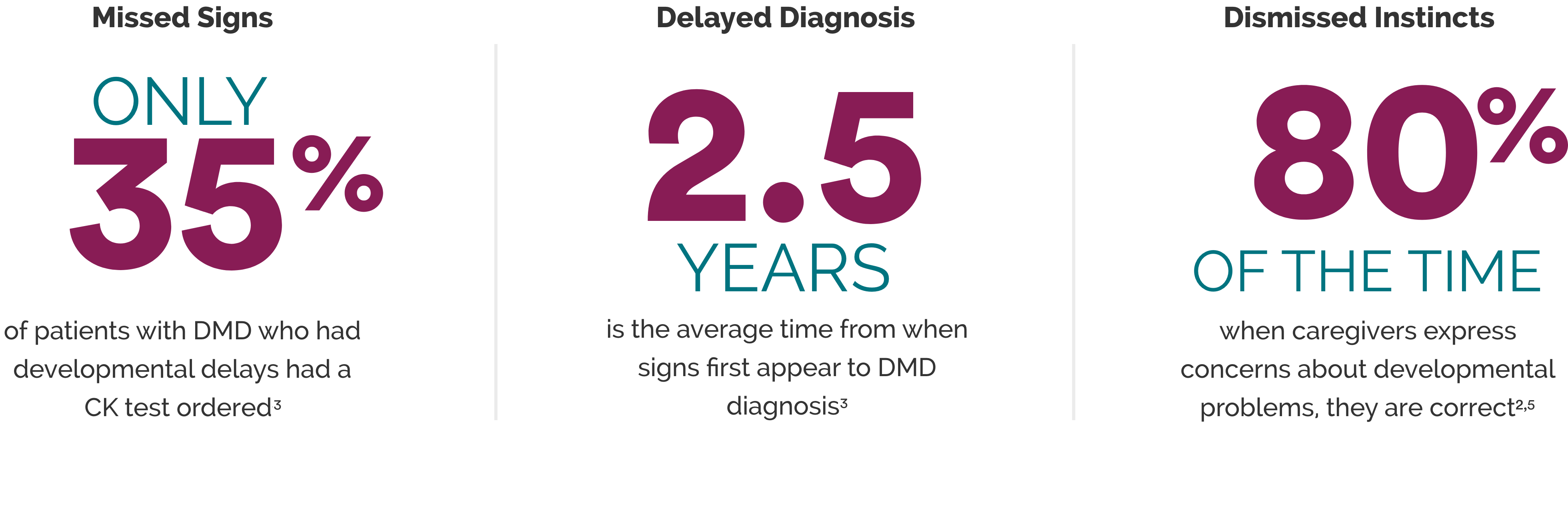
In Patients with DMD, Diagnosis is Often Delayed
Early Diagnosis Is Crucial in DMD
Patients with DMD begin experiencing muscle degeneration at birth.1
While the first signs of DMD may appear as early as 4 months, the average age at diagnosis is between 4 and 5 years.2,3
A delay in diagnosis means some motor skills have already begun deteriorating.4
Why It Matters
Diagnosing DMD earlier will enable patients to access management options, clinical trials, and support networks earlier. It will also allow families to receive genetic counseling, which will help with carrier screening and family planning.2,3
Some treatments and clinical trials may have age restrictions. Diagnosing patients earlier may allow them to participate in more trials or have more therapeutic options.8
If your patient has developmental delays, checking creatine kinase (CK) levels can help determine if a neuromuscular disorder is present.6
The National Task Force for Early Identification of Childhood Neuromuscular Disorders, the AAP,† and the AAFP‡ recommend early CK testing.2,6,7
†American Academy of Pediatrics.
‡American Academy of Family Physicians.
REFERENCES
1. Chen Y-W, Nagaraju K, Bakay M, et al. Early onset of inflammation and later involvement of TGF in Duchenne muscular dystrophy. Neurol. 2005;65:826–834. 2. Lurio JG, Peay HL, Mathews KD. Recognition and management of motor delay and muscle weakness in children. Am Fam Physician. 2015;91:38-44. 3. Ciafaloni E, Fox DJ, Pandya S, et al. Delayed diagnosis in Duchenne muscular dystrophy: data from the Muscular Dystrophy Surveillance, Tracking, and Research Network (MD STARnet). J Pediatr. 2009;155:380-385. 4. van Ruiten HJA, Straub V, Bushby K, Guglieri M. Improving recognition of Duchenne muscular dystrophy: a retrospective case note review. Arch Dis Child. 2014;99(12):1074-1077. 5. Glascoe FP, Dworkin PH. The role of parents in the detection of developmental and behavioral problems. Pediatrics. 1995;95:829-836. 6. National Task Force for Early Identification of Childhood Neuromuscular Disorders website. Accessed on May 4, 2021. https://childmuscleweakness.org/know-the-signs/signs-of-weakness-by-age-for-primary-care 7. Noritz GH, Murphy NA. Motor delays: early identification and evaluation. Pediatrics. 2013;131:e2016-e2027. 8. Aartsma-Rus A, Ginjaar lB, Bushby K. The importance of genetic diagnosis for Duchenne muscular dystrophy. J Med Genet. 2016;53:145-151.

